How can we help you Hear, Speak, and Connect?
Preventive Care
Did you know one in four people aged 20 – 69 show signs of noise induced hearing loss? This form of hearing loss is irreversible and it’s totally preventable!
What’s worse is that the health effects of hearing loss go beyond our ability to hear well. Chronic noise exposure has non-auditory health effects including cardiovascular disease and increased mortality.
Don’t wait until hearing loss affects your quality of life. Be proactive about your health and safeguard your future by preventing the most common and overlooked form of hearing loss.

Your hearing can easily be damaged by sounds over 85 dB. Traffic, loud music, hair dryers, and power tools can all exceed that level. Noise Induced Hearing Loss or NIHL is the most common form of hearing loss. This is a slow and painless process and most people don’t realize when it’s happening.
Reduce noise by 15 – 30 dB with custom made earplugs. We will craft a pair to your ear, ensuring a perfect fit and the best possible sound protection.
Whether you work in loud settings such as a factory, construction site, airport, nursery, bar, or are a frequent traveler, sports enthusiast, hunter, concert-goer; you can protect your hearing health with a pair of high quality, reusable earplugs made just for you.
When water gets trapped inside your ears, it can lead to painful infections. If this happens frequently enough or is left untreated, it can damage the inner ear, leading to hearing loss.
Keep your ears from getting waterlogged while you swim. Our custom fit swim molds prevent water from reaching the inner ear, keeping you and your hearing safe.
If you are a swimmer, kayaker, rafter, paddleboarder, or are prone to ear infections, swim molds are a cost-effective way to ensure your hearing health.
Are you exposed to loud sounds regularly but don’t want to reduce the quality of the sounds you’re hearing? Musician ear plugs may be the answer for you!
With a deeper fit than traditional ear plugs, these specialized plugs keep sound sharp by reducing occlusion (hollow or boomy sounds common in lower quality earplugs). Without causing any muffling or distortion of speech and music, our musician ear plugs give you the freedom to hear what’s important while blocking damaging low to mid frequencies by 20 dB.
The preservation of sound quality make these an excellent choice for band members, DJs, sound engineers, band teachers, referees, athletes, and more.
Audiology Exams
Are you experiencing difficulty understanding conversations, television, or phone calls? Having a hard time hearing birds, children, or your pets? Struggling to know the difference between consonants, for example, “s” and “f” sound the same? Experiencing persistent ringing in your ear or pain associated with noise?
We can help.
When you come in for an evaluation, we will get to the root of why you’re having trouble with your hearing health, then give you the best course of action to ease your symptoms and reclaim your communication skills.
Why get a Hearing Test?
Not all hearing loss is the same and sometimes it’s barely even noticeable to the person experiencing it. Getting a routine hearing test will determine the type and extent of hearing loss you may have.
What to expect
Hearing tests are quick and painless. Our audiologists use a variety of tests and tools to examine the different parts of your ear and determine their health and functionality.
Your audiologist will perform an otoscopy to visually check the inside of your ears. Using a small camera called an otoscope, they will look at your external ear canal and eardrum to check for signs of infection, fluid, or injury.
A tympanometry test will evaluate the function of your middle ear. It measures the movement of the eardrum, volume in the external ear canal, and ear pressure. During this test you will feel a push of air and hear a low tone. You won’t have to provide a response; you’ll just have to sit and stay quiet for a brief moment.
You will have an audiometry evaluation to test your hearing abilities. During this test, you’ll wear headphones or inserts and listen to tones of varying frequencies. Your results will produce an audiogram, a graph that shows how well your hearing performs. We will help you understand where you may be struggling to hear and what treatments are available.
For hearing aid users, we take Real Ear Measurements to determine the optimal settings needed for your specific needs.
What is a Cochlear Implant?
Cochlear Implants are devices designed to replace damaged or ineffective sensory cells in your ear with electrodes that mimic the natural process of hearing. The newly implanted electrodes restore access to sound by creating a new pathway for sound to reach your brain.
Here’s how it works: Sounds from your environment are received and processed through the cochlear implant’s wearable processor. The sounds are turned into electrical impulses and sent to electrodes that are implanted into your cochlea. These impulses stimulate the hearing nerves in your cochlea. The nerves send signals to your brain, giving you the experience of hearing.
Though this is not quite the same as natural hearing, it is a close approximation that your brain can use to understand speech sounds and your environment.
Cochlear Implants are life changing technology. They help prevent social isolation, increase cognitive function, and improve overall health. Studies show that cochlear implants can delay or even reverse cognitive decline, providing both mental and emotional benefits.
We will support you every step of the way and set you up for long lasting success with your implant. Having a cochlear implant will require a commitment to regularly visiting your audiologist, speech pathologist, and/or surgeon for the rest of your life. Your team will be valuable in optimizing your device, giving you the best possible hearing experience. Be sure to choose practitioners you trust who are as committed to your health as you are.
Evaluations
To determine candidacy, we will perform a physical exam on both ears and assess your speech and word recognition. Cochlear implants can be utilized in both or just one ear.
Just like in a routine hearing examination, we will test your hearing thresholds and plot them on an audiogram, with and without your hearing aids. This will help us determine the type and degree of hearing loss.
We will discuss your difficulty in communication and the impact it has on your life as well as challenges that may arise from using cochlear implants and what lifestyle changes you may have to face.
Additionally, we will discuss your lifestyle factors to find the best solution for you. Things to consider are wearing options, water resistance, smartphone connectivity, upgradability, and ongoing care. We’ll set expectations for life after the implantation and come up with a long-term plan for care.
After your Implant Surgery
A couple weeks after your implant, your audiologist will examine your implant site to ensure the healing process is going normally.
We will turn on your device and make an initial assessment of what you’re able to hear, adjusting the settings to give you the clearest sounds possible. We will discuss basic device use, ensure comfort, and address any concerns you have. You will visit your audiologist regularly, especially in the first 6 months after implantation. These visits will consist of optimizing your device settings, confirming consistency of device use, addressing sound quality issues, practicing hearing exercises, checking that your device is working properly, and evaluating your progress on understanding speech.
To give you the best possible outcome with your cochlear implant device, your audiologist will make adjustments to the input of the electrodes based on how you experience sound and how well you’re able to recognize and understand speech sounds. Adjustments will be made to both the softest sounds you’re able to hear and the loudness of incoming sounds. This process is called mapping and will be done periodically during the first few years of using your implant to find the perfect settings for you and your lifestyle. After each mapping, we’ll retest your speech perception.
If you consistently wear your implants and participate in speech and hearing practice, you are likely to see great results within the first couple months.
Benefits of Ongoing Care – Aural Rehab
Hearing is a learned behavior. It takes time and therapy to get used to living with a cochlear implant. The first couple months of cochlear implant use may be disappointing and difficult. Sounds may come across as unfamiliar, mechanical, and/or unpleasant. This is normal and will change over time as your brain adjusts to hearing with the implant. Your brain needs to learn how to apply meaning to the signals it’s receiving.
We have programs designed to support you through this initial adjustment process and to continue the intentional practice of using your device as time goes on. Our Aural Rehab program provides hearing exercises that challenge your brain in quiet as well as background noise to learn to distinguish between certain sounds.
How hearing works
The act of hearing is not limited to our ears. It involves the brain identifying and processing sound stimuli to understand the environment.
When you are tuned in and purposefully trying to make sense of what you are hearing, or actively listening, neurons fire in areas of the brain responsible for sound detection and recognition. The way these neurons fire shapes the way your brain perceives sound input, essentially “choosing” which sounds to pay attention to and giving them meaning. Your brain will create deeper pathways to the sounds it considers important while lessening the ability to detect the sounds it does not.
Can hearing loss be cured?
It’s important to have realistic expectations when living with hearing loss. There is no device or training program that can fully restore hearing to its pre-loss level. Therefore, the focus of our aural rehabilitation program is to improve your ability to function and participate in your daily life. Our goal is to help you adjust to living with hearing loss, minimizing the impact it has on your quality of life. We do this by helping you become adept at using your hearing aids or cochlear implants, teaching you to manage sensory input, and improving your effectiveness in communication.
What is Aural Rehab?
In aural rehab, we work with the entire hearing system, from your ears to your brain. This holistic approach allows us to improve your ability to understand your sound environment. When people experience hearing loss and are fitted with a new hearing aid or cochlear implant, some sounds that used to be familiar may sound strange or incomprehensible. For this reason, using hearing aids or cochlear implants takes practice.
The goal of aural rehabilitation is to retrain your brain to understand the sound input it’s receiving. Aural rehab consists of monthly listening sessions that last for about 30 – 60 minutes. You’ll do listening exercises to help your brain make sense of common sounds, including speech sounds, in a low stress environment with immediate feedback. These exercises build the neural pathways that can reduce your perception of hearing difficulties.
Benefits from this therapy are usually quick, with noticeable results being seen after just one session. Similar to how you would build a muscle, following a consistent, intentional program will provide significant, long-lasting results. Aural rehab can make it easier to navigate conversations and reduce interpersonal stress when difficulties around communication occur, giving you the ability to stay present and participate in social activities.
What is that ringing in your ears?
Tinnitus can be a deeply uncomfortable experience. The feeling of a persistent ringing, buzzing, or hissing in the ear can disrupt your daily life and leave you feeling overwhelmed, stressed, or exhausted.
But where does this sound come from? Tinnitus most often happens when certain hair cells in your ear become damaged and can no longer balance the sound signals your ear is receiving. This causes your brain think there is sound input when you are in quiet environments.
Can Tinnitus be cured?
Though we can’t reverse the damage to your hair cells, we can teach you techniques to help manage and minimize your brain’s response to the signals it’s receiving.
Using Sound Therapy, Re-Training Therapy, and Progressive Tinnitus Management, we will enlist the help of your limbic and autonomic nervous systems to help you gain control of your perception and ultimately change the experience from a negative to a neutral one.

Speech Therapy
Do you or a loved one struggle putting words together, communicating ideas, or comprehending what others are saying? We treat children and adults with language delays and other speech disorders, as well as people who experience speech and language impairments caused by stroke, brain injuries, or illnesses.
With speech disorders, it is also common to have problems with memory, attention, perception, and comprehension. We focus on building skills related to cognitive-communication disorders, early language development, swallowing disorders, sound production, comprehension, fluency, clarity, and expression.
What is a Functional Speech-Language Disoder?
Functional speech-language disorders often have no known cause and don’t always indicate abnormalities with your child’s hearing, muscles, or perception. These disorders usually show up in childhood and can consist of abnormalities in muscle usage or linguistic aspects, affecting the rhythm, pitch, and intonation of speech. People who are affected by functional speech disorders may speak with an unusual quality, making sounds that are hoarse, raspy, breathy, strained, or weak.
Functional speech-language disorders can lead to social anxiety and avoidance behaviors as well as contribute to low self esteem due to social stigmatization and occupational discrimination.
Our Speech-Language Pathologists can assess your child to determine whether they are experiencing an articulation disorder, another type of speech-language issue, or sensory issues like hearing impairment. Early treatment can help your child overcome any speech difficulties and learn to speak comfortably and effectively.
Articulation
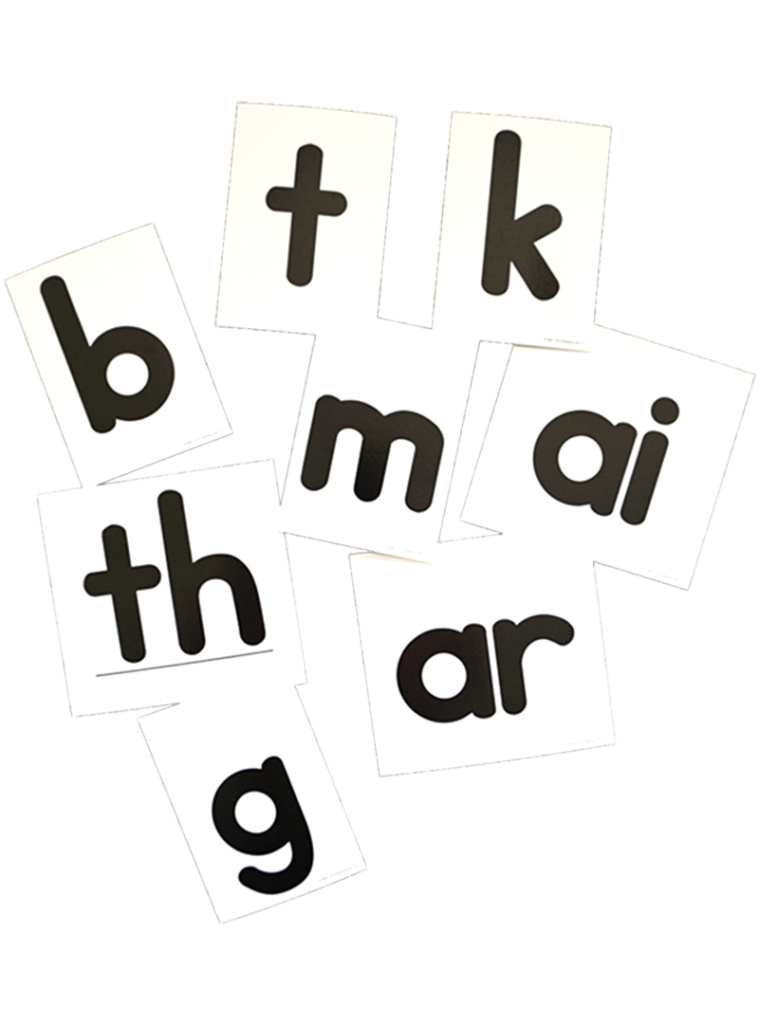
With articulation disorder, children may have trouble coordinating their flow of speech and struggle with the placement of their tongue, lips, palate, teeth, and jaw. This usually shows up in four ways:
Substitution: Consistently using one sound in place of another. For example, they may use the w sound instead of r, use an s or f sound instead of th, or use a t instead of ck.
Omission: Completely leaving out certain sounds or shortening words. Examples include saying ool instead of pool or school, saying cu instead of cup, or saying at for hat.
Distortion: Using an atypical sound in place of certain speech sounds. This would look like a nasally produced p that sounds more like an m or an s that sounds fuzzy. Lisps are a common form of distortion.
Addition: Adding syllables or sounds to words. Examples include saying puhlay instead of play, or saying dogah instead of dog.
SLPs can help your child re-learn how to make certain speech sounds, control muscles involved in speech production, recognize which sounds need adjustment, and practice sound formation in different words.
Articulation milestones:*
- By age 3, a child should be able to pronounce all vowels and the p, b, m, h, and w sounds.
- At age 4, the sounds d, t, k, g, f, n, ng, and y should appear.
- At about 6, you should see proper use of the sounds s, z, l, v, and sh.
- By age 7, children have mastered j, ch, and th sounds
- And by age 8, use of r and zh is acquired.
*These speech markers are based on English speaking children with no regional accents. The use of multiple languages and influence of regional dialects may alter the formation of certain speech sounds. In those cases, there is no need for concern or therapy.
Phonology
While articulation disorders affect the pronunciation of one sound and tend to be motor based, phonological disorders refer to the misapplying of patterns of sounds and an incomplete understanding of the rules around the meaning of sounds. It’s normal for young children to use these phonological short cuts when learning adult speech but, if your child continues to mispronounce words longer than their peers, it can indicate a phonological issue. Phonology disorders can show up in a variety of ways.
Fronting: Replacing sounds made with the back of the tongue for those made with the front of the tongue. For example, saying tar instead of car or date instead of gate. The process of fronting usually
disappears before age 4.
Stopping: When a child is unable to produce hissing or sounds that create a stream of air such as the s, sh, ch, th, j, z, or f they may use a stop consonant in it’s place. Stop consonants are p, b, t, d, k, and g. Stopping results in children saying pun instead of sun or saying top instead of shop. This process is usually eliminated between the ages of 3 and 5.
Final Consonant Deletion: Completely dropping the last syllable of multi-syllabic words or the last consonant of one syllable words. This may look like a child saying wa for water, or bie instead of bike. Final consonant deletion usually disappears by age 3.
Cluster Reduction: Leaving out one consonant in words that contain 2 or more consonants together. Your child may drop the s in spill resulting in pill, or the r in tree to produce tee. This process is usually gone by age 4.
With phonological disorder, children may be able to produce individual sounds correctly but struggle when trying to put sounds together. Your child may be able to make the C sound on its own but, when your child tries to say a word that starts with C, they may use a T sound instead.
SLPs can improve your child’s intelligibility by helping them recognize the sounds that need adjustment, understand the differences in meaning between similar sounds, teaching your child how to make certain speech sounds, and practicing proper formation of words.
Fluency
Fluency disorders affect the flow and cadence of speech. People experiencing fluency issues may take frequent pauses while talking, repeat sounds, stretch sounds out, or have an unusual rhythm of speech. While everyone experiences trouble with fluency at times, people with the disorder are affected on a regular basis which causes a disruption in their life. The two most common types are:
Stuttering: Categorized by frequent repetitions of sounds and syllables or the stretching out of consonants.
Cluttering: Categorized by rapid rate of speech, shoving together of words, skipping over syllables, and/or omission of word endings.
Fluency disorders can co-occur in people who also experience auditory processing disorder, ADHD, Tourette syndrome, are on the autism spectrum, or have learning disabilities.
Treatment for fluency disorders by SLPs can result in increased effectiveness of communication, increased self-confidence, and improved social engagement.
What is a Cognitive Language Disorder?
Sometimes speech-language issues have a physical or motor origin, but other times, they’re caused by a disconnect in the brain. People who experience cognitive related language issues may have difficulty following conversation, remembering information, following directions, and/or putting their thoughts into words. This can affect their ability to manage daily tasks. Cognitive Language Disorders can show up in childhood as a developmental delay, or later in life due to neurological disease or trauma.
Aphasia
Aphasia is a condition that affects your ability to communicate thoughts and understand language. Adults who experience brain injuries due to stroke, Alzheimer’s disease, tumors, or physical trauma may have difficulties with the language parts of their brains. People who experience aphasia may struggle to recall words they want to say, mix words up, use the wrong word, and struggle recognizing an object by its name. By improving language skills and/or finding alternative ways to communicate, our Speech-Language Pathologists (or SLPs) can help people experiencing aphasia participate more fully in life.
Developmental Language Disorder
Developmental Language Disorder is usually noticed when a child is a late talker and having trouble keeping up with their peers in language development. Usually the cause is unknown and is not related to intelligence or speech ability, but can exist alongside other conditions such as autism and Down’s syndrome. Language Disorders affect a person’s ability to express themselves and/or understand things that are spoken to them. This can interfere with learning by affecting their speaking, writing, reading, and listening abilities.
With an expressive language disorder, there is no problem with pronunciation or speech capabilities. Rather, people struggle to organize their thoughts into words. Children experiencing it may use words incorrectly, use limited vocabulary compared to their peers, struggle to form sentences, and have trouble reading and writing.
Receptive language disorders have to do with understanding what others say. Children who experience this disorder have trouble processing the meaning of spoken and written language. They may not understand what people are saying to them and struggle to follow directions or connect with others.
Some children may show signs of only one of these disorders, while others experience both. Developmental Language Disorders can be frustrating for the child experiencing them and they may act out or avoid interactions altogether. Our Speech-Language Pathologists can diagnose these disorders and help children fill in the gaps of grammar and word usage while developing social communication skills.
If you are concerned your child is behind their peers in speech and language abilities, check the American Speech-Language-Hearing Association’s chart of speech milestones by age to determine if you should talk to your doctor:
What are Motor Speech Disorders?
It takes the coordinated effort of about 100 muscles in your lips, tongue, throat, chest, and neck to produce speech. Many of the same muscles are responsible for swallowing food and drink. If these muscles are weak or not communicating with the brain properly, people may experience difficulty making speech sounds or struggle to eat and drink.
Impairments to these muscles can be caused by developmental disabilities or by damage and illnesses that affect the nervous system such as stroke, Parkinson’s disease, multiple sclerosis, ALS, cerebral palsy, or Alzheimer’s. The effect these disorders have on the muscles involved with speech can be mitigated by Speech-Language Pathologists.
Apraxia
Apraxia is a condition that can affect both children and adults. Apraxia happens when the brain and muscles don’t communicate properly. Though there is no muscle weakness, people experiencing apraxia struggle with moving their muscles to produce speech. With apraxia, people may not always say words the same way every time, may change or distort sounds, struggle with longer words, or have difficulty with fine motor skills. Our SLPs can help improve coordination of muscles to produce desired sounds using visual, listening, and touch cues.
Dysarthria
Dysarthria is a speech disorder characterized by muscle weakness. The tongue, larynx, and surrounding muscles can become paralyzed or weakened by damage to or disorders of the brain and nervous system. People who experience dysarthria can struggle to form and pronounce words. Someone with dysarthria may have slurred speech, talk either too fast or too slow, or have trouble moving their tongue, lips, and jaw. The quality of their voice may sound robotic, hoarse, breathy, or nasally.
Our SLPs test speech and language abilities through a series of movement and language tasks. The SLP will watch how the muscles in your mouth, lips, and tongue move when speaking as well as check your breathing ability. They can teach techniques to speak more clearly, improve articulation, strengthen muscles, and provide supplemental ways of communicating. They will also determine if any additional support is needed with understanding language.
Dysphagia
Dysphagia refers to difficulty swallowing food or drink. Problems can arise with sucking, chewing, and moving food or liquid into the throat. People who experience dysphasia may feel the urge to cough while swallowing, feel as if food is sticking in their neck/chest, or have pain when swallowing. People with dysphasia may also experience recurring reflux, frequent lung infections from food entering the airway, or poor nutrition due to avoidance of food.
Our SLPs can give exercises to strengthen the muscles used for swallowing as well as teach posturing techniques to minimize unpleasant sensations and keep food moving along. They will also help identify problem foods and give tips on changing the consistency of foods that aggravate swallowing difficulties.
What is a Resonance Disorder?
The vocal tract consists of our nasal cavity, oral cavity, throat, and vocal cords. This is the area where speech sounds are made. When we talk about resonance we’re referring to the tone and quality of sound vibrations produced from our vocal folds as they pass through our vocal tract. In other words, vibrations resonate through our oral and nasal cavities to produce the vowel and consonant sounds we’re familiar with.
During normal resonance, the soft palate and the walls of the throat come together to form a seal that separates the oral and nasal cavities. This mechanism, dubbed the velopharyngeal valve, directs airflow to the oral cavity during speech. When this valve has structural irregularities or otherwise doesn’t function as a tight seal, it can cause a resonance disorder. A cleft palate is a common structural cause of this disorder.
Our Speech-Language Pathologists can help identify what may be causing a resonance issue and work with you to mitigate the impact of this disorder by building effective communication skills.
Hypernasality
A condition called hypernasality happens when excessive sound comes from the nose. Someone experiencing hypernasality may sound high-pitched or like they’re speaking through their nose. As air escapes through the nose, pressure cannot build up in the mouth and the pronunciation of consonants can become weak. A child may replace consonants with abnormal speech sounds such as using the sound uh in place of g.
Hyponasality
A condition known as hyponasality occurs when there is not enough sound coming through the nose. This can be due to a blockage in the nasal cavity or throat. Common causes include enlarged tonsils, enlarged adenoids, or obstruction in the nose. Someone experiencing hyponasality may sound “stopped up” or congested. A child may mispronounce nasal consonants making m sound like b or the letter n sound like d.
Hearing Aids
Your hearing is as unique as you are. Our trained, licensed audiologists will program and fit your hearing aids to meet your specific needs.
We’ll give you all the tools and knowledge you need to be successful with your hearings aids. We’ll train you to use them effectively in different environments, connect them to your smart devices, and troubleshoot any problems that may arise.
We work with the top hearing aid manufacturers to provide the highest quality products with state of the art technology at reasonable prices.
Unbundled Hearing Aid Prices
High End
-
Best noise suppression + noise cancellation
-
Up tp 8 kHz bandwidth
-
Best speech understanding
-
Near instant processing
-
Automatic environmental adjustments
Mid Level
-
Better noise suppression
-
Up to 6 kHz bandwidth
-
Better speech understanding
-
Fast processing
Entry Level
-
Good noise suppression
-
Up to 4 kHz bandwidth
-
Good speech understanding
Not ready to commit to purchasing hearing aids?
We’ll let you test drive a pair! Ask about our demo or rental program.

Ongoing Care
We want you to set you up for success with your new hearing aids, making sure they work for your lifestyle. When you purchase a set of hearing aids with us, you will also receive the following services for up to 3 years at no extra cost to you:
Follow-up visits
Hearing tests + fine tuning of hearing aid settings
Real Ear Measurements
Tailored, one-on-one Aural Rehabilitation program
Cleanings and repairs
Optional Add Ons
In addition to our standard hearing aids, you can opt for a rechargeable battery station that doubles as a disinfector. We also supply warranties to protect your investment should something unexpected happen.
Rechargeable battery – $200
Loss and Damage Warranty – $250 per hearing aid
Optional Add Ons
In addition to our standard hearing aids, you can opt for a rechargeable battery station that doubles as a disinfector. We also supply warranties to protect your investment should something unexpected happen.
Rechargeable battery – $200
Loss and Damage Warranty – $250 per hearing aid
Sign up for our Newsletter
Receive the latest information directly to your inbox.
